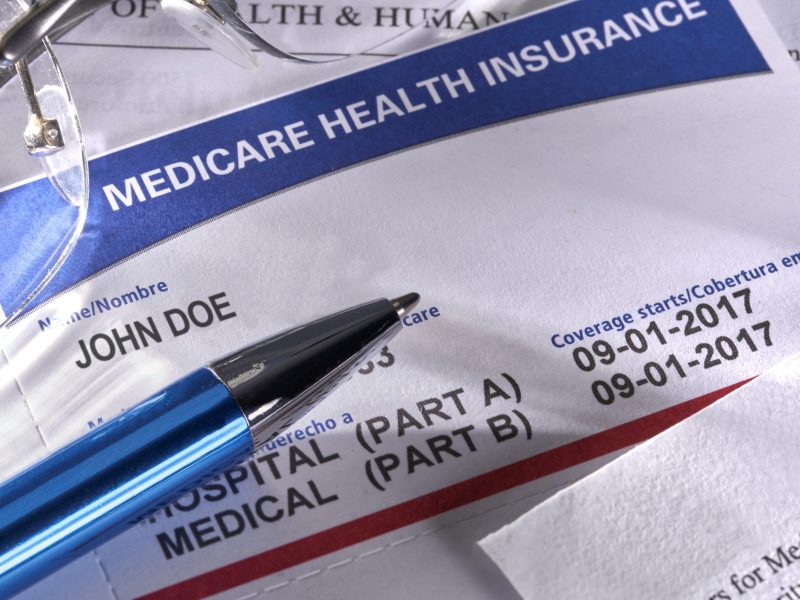
Medicare Advantage, the $450-billion-a-year system in which private insurers oversee Medicare benefits, grew out of the idea that the private sector could provide healthcare more economically than the United States federal government. Well, this idea has proven to be anything but economical. The Wall Journal has reviewed Medicare data and has discovered that instead of saving taxpayers money, Medicare Advantage has added tens of billions of dollars in costs.
Medicare Advantage allows insurers to add diagnoses to ones that patients’ own doctors have submitted. Medicare gave insurers that option so they could catch conditions that doctors neglected to record. But fraud seems to be the only result in this plan. After paying doctors for access to patient records and rewarding the patients who agree to home visits with gift cards, private insurers involved in the government’s Medicare Advantage program made hundreds of thousands of questionable diagnoses that triggered extra taxpayer-funded payments. How do we know these diagnoses are questionable? The Journal’s analysis found that insurers have pocketed $50 billion from Medicare for diseases no doctor treated.
To protect insurers from the risk of winding up with sicker-than-average patients, in 2018 the government allowed bigger payments for certain serious health conditions. Conditions such as diabetic-cataracts, HIV, and Emphysema. Care to guess which conditions skyrocketed amongst Medicare recipients between 2018 and 2021? Diabetic-cataracts, HIV, and Emphysema. Seems suspicious? In response, a spokeswoman for the Centers for Medicare and Medicaid Services said the agency was making changes that would continue to ensure “taxpayer dollars are appropriately spent.” CMS even claimed the changes they are making shows it is a “good steward of taxpayer dollars.” Apparently spent on fraud it looks like. Instead of fixing a system based on diagnosis codes, Medicare administrators are currently making the list (and checking it twice) of diseases for which insurers earn higher payments in 2026. Some of the most heavily used diagnoses, including diabetic cataracts, will pay less or nothing extra. New diagnoses, including asthma, were added to the list of conditions warranting extra payments. So, place your bets now that there is going to be an uptake in asthma diagnoses next year.
Shout out to The Wall Street Journal. Excellent journalism.
Today’s Fraud of The Day is based on article “Insurers Pocketed $50 Billion From Medicare for Diseases No Doctor Treated” published by The Wall Street Journal on July 9, 2024.
Gloria Lee was perplexed when the phone calls started coming in from a representative of her Medicare insurer. Could a nurse stop by her Boston home to give her a quick checkup? It was a helpful perk. No cost. In fact, she’d get a $50 gift card.
After several such calls in 2022, Lee agreed. A nurse showed up, checked her over, asked her questions, then diagnosed her with diabetic cataracts.
Senior Director of Strategic Alliances
LexisNexis Risk Solutions - Government
LexisNexis Risk Solutions - Government
Related Articles
Get Your Fraud Fix!
Five days a week wake up to the most current fraud article in your inbox
Contact Us
Thank you for your interest in Fraud of the Day. For more information, please complete the following form.
To receive the most current fraud articles direct to your inbox, click the Subscribe button above.
"*" indicates required fields