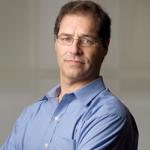
Every minute counts when it comes to submitting claims to government healthcare programs. A primary care doctor in Webster City, Iowa was quick to tally the minutes he spent with his patients at multiple nursing facilities (and multiply that number by seven). After nearly five years of falsifying claims, all those minutes added up to some pretty hefty reimbursements from the government. That means the doctor will be counting the long, tedious minutes while serving time in prison for carrying out a healthcare fraud scheme that bilked the government out of more than $300,000.
Here’s a little background information for you: The Northern Iowa primary care doctor used the most intensive and expensive claim codes for routine visits he made to nursing home patients.
Investigators found through in-person and video surveillance that the doctor spent under five minutes with each patient he visited. But. he billed more than 93 percent of his nursing home visits under a higher paying claim code. (The more expensive code required him to spend 35 minutes at each patient’s bedside and on the patient’s facility floor or unit.) Medicare reimbursed the doctor for $94 per claim. (If the doctor had been honest, he would have only received $32 per routine visit.)
In 2016, the doctor from Iowa received a warning letter stating that his billing patterns were significantly more expensive than other doctors. Fast forward two years to when the doctor submitted sworn statements to the U.S. Attorney claiming he was visiting patients for 35 minutes each. He backed up his sworn statement with re-created treatment notes. (He had to re-create them because he shredded all notes for nursing home patients immediately after he billed the government for the services. Uh, that’s just bad records management to say the least.)
This doctor was a busy man. He was the medical director of two nursing homes, county coroner, and he also evaluated workers’ compensation claims for a Webster City employer. Over nearly five years, he submitted 1,140 fake claims to Medicare which paid him $107,980.59. He also received $9,218.73 in unjustified payments from Medicaid.
In addition to being sentenced to two months in prison, the fraudulent doctor from Iowa will have to pay more than $316,000 to settle False Claims Act allegations. (Let’s hope that while serving out every one of his 86,400 minutes in prison, this fraudster will make every minute count.)
Today’s Fraud of the Day comes from a Department of Justice press release, “Northern Iowa Doctor Sentenced to Federal Prison for Making False Statements and Will Pay More Than $315,000 to Resolve False Claims Act Allegations Relating to Nursing Facility Residents,” released on January 16, 2020.
Dr. Joseph X. Latella, a primary care doctor in Webster City, Iowa, was sentenced today to two months in prison and to pay a fine after previously pleading guilty to making false statements related to health care matters. Dr. Latella has also agreed to pay $316,438.96 to resolve False Claims Act allegations relating to claims he submitted for routine visits for nursing facility residents between January 1, 2014, and November 30, 2018. The United States alleged that Dr. Latella submitted claims to Medicare and Medicaid for the most intensive and expensive claim code for such visits when, in fact, he was not performing services sufficient to justify use of that code.
Dr. Latella admitted in a plea agreement that, in June 2018, the United States Attorney for the Northern District of Iowa was conducting a civil investigation about concerns that Dr. Latella was “upcoding” claims submitted to Medicare and Medicaid and billing for more intensive visits with patients at Webster City area nursing homes than he had performed. The United States Attorney’s investigation indicated that Dr. Latella was billing over 93% of his nursing home visits to Medicare under the most intensive and expensive claim code. For these claims to be valid, a doctor typically must spend 35 minutes at the patient’s bedside and on the patient’s facility floor or unit. Medicare paid more than $94 for these claims, but would only have paid no more than $32 if the least expensive claim code, for routine ten minute visits, had been billed. In July 2016, a Medicare contractor sent Dr. Latella a letter warning him that his billing patterns were significantly more expensive than other doctors.